This website uses cookies so that we can provide you with the best user experience possible. Cookie information is stored in your browser and performs functions such as recognising you when you return to our website and helping our team to understand which sections of the website you find most interesting and useful.

Contact Lenses as Ocular Prosthetic Devices after Eye Surgery
Contact lenses, once perceived merely as vision correction tools, have evolved into fascinating ocular prosthetic devices. This article delves into their definition, functions, and their impact on individuals globally.
Understanding Ocular Prosthetic Devices:
An ocular prosthesis, synthetic eye, or artificial eye is a craniofacial prosthesis designed to substitute a missing natural eye after undergoing procedures such as enucleation, evisceration, or orbital exenteration. Now to anyone who does not understand enucleation, evisceration and orbital exenteration, the following shares more light:
- Enucleation:
- Enucleation is a surgery where the entire eyeball is removed. It’s done in serious cases, like severe eye injuries or advanced eye diseases.
- Evisceration:
- Evisceration means taking out the insides of the eyeball, leaving the outer part. This is done when the inner part needs fixing, but the outer look remains.
- Orbital Exenteration:
- Orbital exenteration is a complex surgery where not only the eyeball but also some surrounding tissues are removed. It’s usually done in advanced cases of eye cancer.
The prosthetic device is designed to be placed over an orbital implant and positioned beneath the eyelids. While commonly known as a glass eye, the ocular prosthesis typically adopts the form of a convex shell and is crafted from medical-grade plastic acrylic. Some contemporary ocular prostheses are manufactured using cryolite glass.
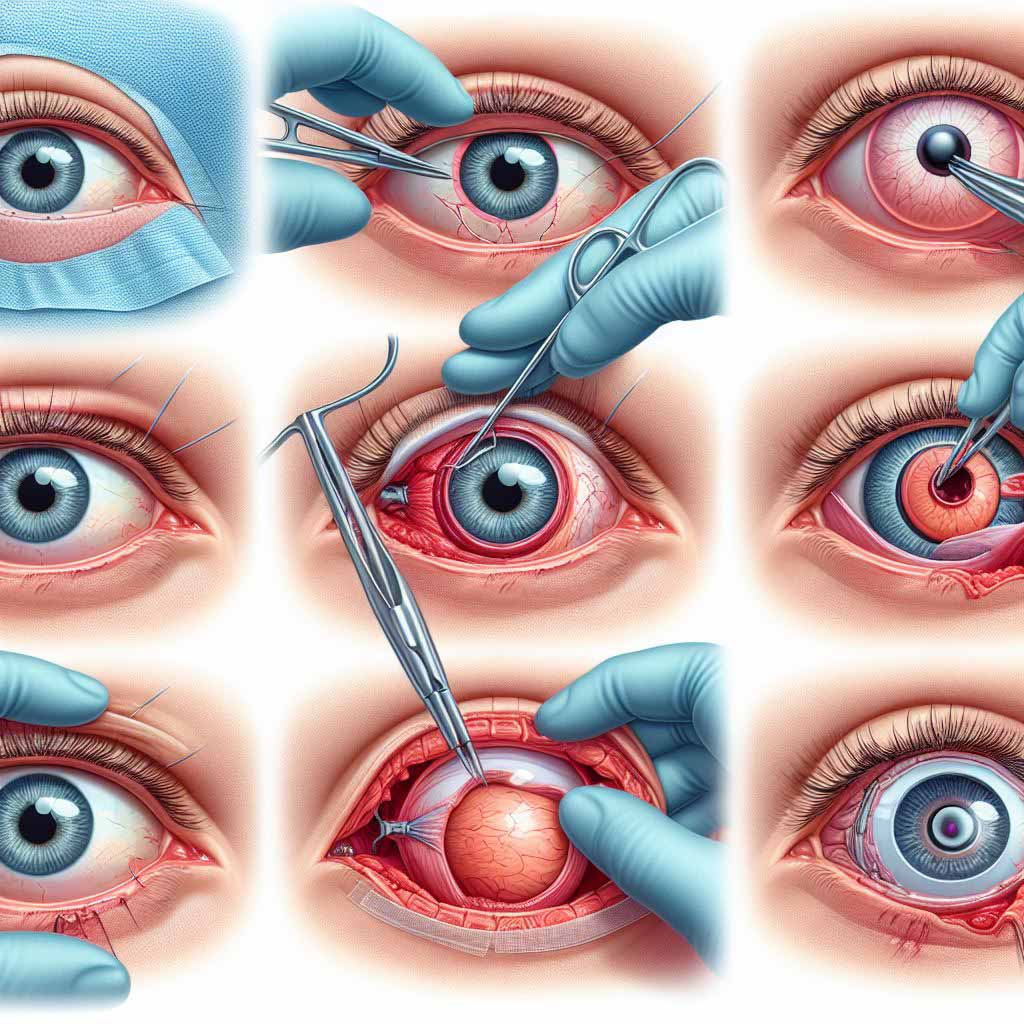
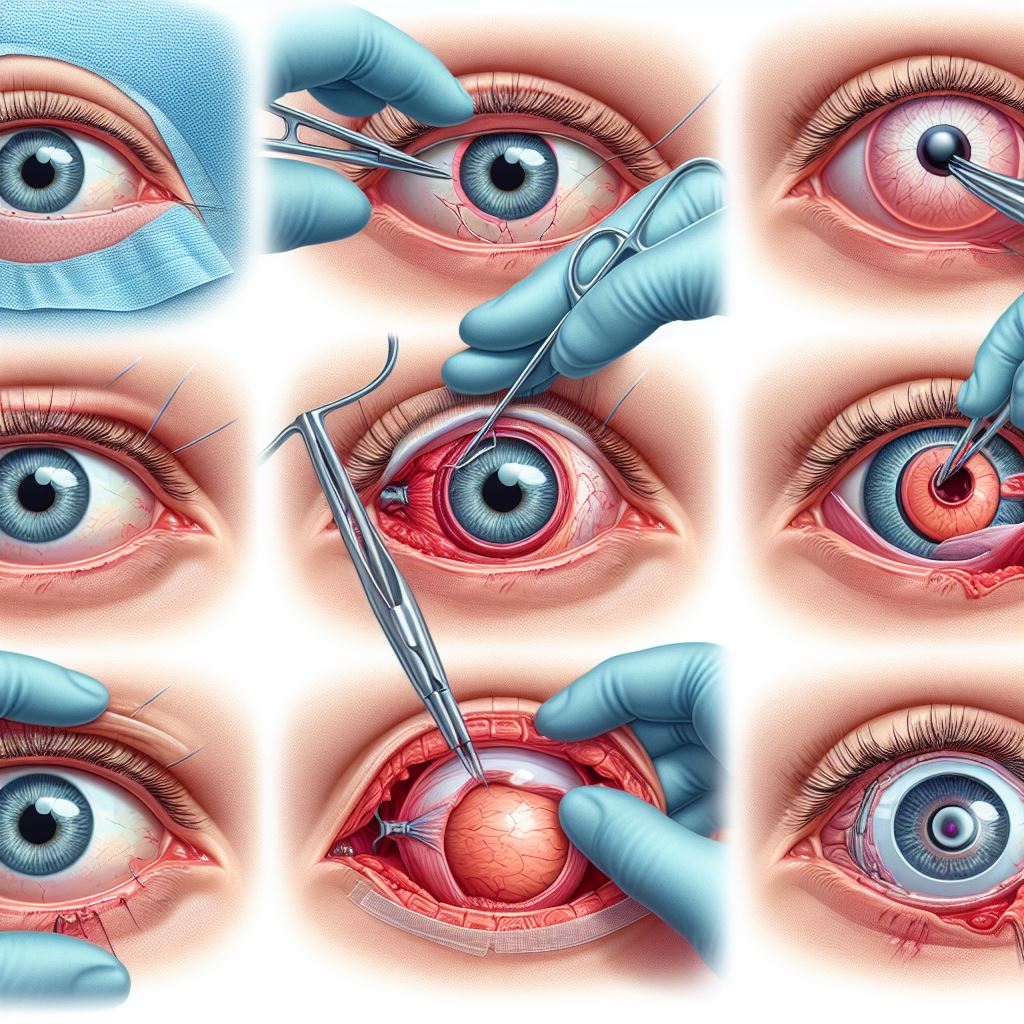
How Prosthetic Eye Surgery is Done

Prosthetic Eye Surgery is a relatively swift procedure, often concluding within an hour. Whether it’s enucleation or evisceration, the surgical process involves inserting an implant into the vacant eye socket following the removal of targeted materials.
The details of the surgery vary based on the specific procedure chosen. In the case of enucleation, where the entire eye is removed, the surgeon meticulously sews the eye muscles to the implanted structure. Conversely, in evisceration, where more eye material is retained, including the sclera and attached muscles, this extensive sewing isn’t necessary.
To aid in the healing process and provide a temporary structure until the placement of a more permanent prosthetic, a placeholder conformer is positioned over the implant. This dual-purpose conformer supports the healing of the eye socket and serves as a temporary solution until the patient is ready for the placement of a prosthetic eye, typically around two months post-surgery.
It’s crucial to note that the surgical approach is tailored to the individual’s needs and the chosen procedure, ensuring a comprehensive and personalized path towards recovery and the eventual use of an ocular prosthesis.
Top Ocular Prosthetic Devices and their Features.
| Name | Material | Features | Description |
|---|---|---|---|
| Acrylic Spheres | Polymethyl Methacrylate (PMMA) | Transparency, good tissue compatibility, nonintegrated design. | Acrylic spheres made from PMMA offer transparency and tissue compatibility, featuring a nonintegrated design. |
| Glass Eyes | Traditional glass | Historical use, fragility, replaced by modern materials. | Traditional glass eyes, historically used but replaced by modern materials due to fragility. |
| Silicone Spheres | Soft, flexible silicone | Comfortable, nonintegrated design, flexibility. | Silicone spheres provide comfort with a nonintegrated design and flexibility. |
| Hydroxyapatite Implants | Porous hydroxyapatite | Spherical, fibrovascular ingrowth, covered with exogenous material. | Hydroxyapatite implants offer fibrovascular ingrowth with a spherical shape, covered with exogenous material. |
| Porous Polyethylene (PP) Implants | Porous polyethylene | Firm, malleable, direct suturing of muscles, no covering required. | Porous polyethylene implants are firm, malleable, allowing direct suturing of muscles without the need for covering. |
| Bioceramic Implants | Aluminium oxide | Biocompatible, low friction, durable, various shapes and sizes. | Bioceramic implants made of aluminium oxide are biocompatible, low-friction, durable, and available in various shapes. |
| Conical Orbital Implants | Various, including PMMA | Unique conical shape, channels for rectus muscles, multiple sizes. | Conical orbital implants feature a unique shape, rectus muscle channels, and come in various sizes. |
| Multipurpose Conical Orbital Implants (MCOI) | Custom materials | Anatomic shape, reduced postoperative issues, improved motility. | MCOIs are custom-made with an anatomic shape, addressing postoperative issues and enhancing motility. |
| LCD-Simulated Pupil Devices | LCD-based technology | Simulation of pupil size based on ambient light, improving realism. | LCD-based devices simulate pupil size based on ambient light, enhancing the realism of artificial eyes. |
| Pegged (Motility Post) Implants | Titanium, hydroxyapatite, or PP | Enhanced motility, ball-and-socket joint, peg for direct transfer. | Pegged implants feature enhanced motility, a ball-and-socket joint, and a peg for direct transfer of implant motility. |
Global Usage Statistics:
The global utilization of contact lenses has witnessed a remarkable surge in recent years. Practitioners like Kaitlin Morrison, with expertise in prosthetic soft contacts, have played a pivotal role in making these devices more accessible. Comprehensive eye doctors have championed their use, addressing diverse eye conditions and ensuring a good fit for wearers worldwide.
Diverse Applications:
Patients with pacified corneas, sparse iris diameters, or scarred corneas find solace in the tailored solutions offered by contact lenses. For individuals facing challenges in normal life, such as finding employment or coping with disfigurements, these lenses become more than visual aids; they become confidence boosters.
Innovations in Design:
Colored contact lenses, once considered a niche, are now a mainstream option. Matt Geller from Scottsdale, Arizona, emphasizes the role of these lenses in providing customizable solutions. They not only disguise differences but also offer an opportunity for self-expression, especially for those with congenital iris disfigurements.
Overcoming Stigmas:
The topic of prosthetic soft contacts is seldom discussed openly, but understanding their significance can empower patients. The lens market has witnessed a surge in innovative designs, making these devices more mainstream and contributing to the overall well-being of wearers.
Enhancing Lives:
Patients with larger scars or more significant challenges find that contact lenses can be life-changing. The broader selection process, including considerations for scarred corneas, offers tailored solutions. Through the lens basics, wearers feel a bit ostracized from society, but the advancements in this field are making these lenses more widely accepted.
In conclusion, the field of ocular prosthetic devices, particularly contact lenses, has come a long way. From addressing minor things like iris disfigurements to providing customizable, confidence-boosting options, these lenses offer more than meets the eye. As we continue to learn and show empathy, the lens market will keep making strides in specialized offerings, contributing to the well-being and confidence of individuals around the world.
History of Ocular Prosthesis:
- Ancient Evidence: A woman in Shahr-I Sokhta, Iran, had a bitumen paste artificial eye around 2900–2800 BC, adorned with gold.
- Roman and Egyptian Practices: Priests in ancient Rome and Egypt crafted artificial eyes from painted clay in the fifth century BC.
- Venetian Evolution: In the 16th century, Venetians shifted from gold to glass, refining their methods. Parisians and Germans later dominated the industry.
- Shift to the United States: Due to World War II, the U.S. pioneered acrylic plastic artificial eyes when German glass eyes became unavailable.
Limits of Realism in Artificial Eyes:
- Pupil Mobility Challenges: Enhancing artificial eye appearance faced challenges due to immobile pupils.
- Technological Innovation: Recent advancements, like LCD-based devices simulating pupil size, address immobility challenges.
Implant Types and Chemical Construction:
- Diversity of Implants: Implants vary in shape, stock vs. custom, porosity, and chemical composition.
- Nonintegrated Implants: Introduced around 1976, including acrylic, glass, and silicone spheres with no direct attachment to the artificial eye.
- Polymethyl Methacrylate (PMMA): A widely used transparent thermoplastic (acrylic) for nonintegrated implants due to good tissue compatibility.
Types of Porous Implants:
- Hydroxyapatite (HA): Spherical implants allowing fibrovascular ingrowth, despite needing covering material like sclera.
- Porous Polyethylene (PP): Introduced in 1989, firm and malleable, enabling direct suturing of muscles without extra steps.
- Bioceramic (Aluminium Oxide): Introduced in 2000, biocompatible with good outcomes and less exposure risk.
- Conical and Multipurpose Conical Orbital Implants: Unique shapes offering improved anatomical replacement and reduced postoperative issues.
- Pegged (Motility Post) Implants: Introduced in hydroxyapatite, enabling a ball-and-socket joint for improved motility, later extended to porous polyethylene.
Frequently Asked Questions
Functionality and Purpose
Q: What is the primary function of an ocular prosthesis?
A: Ocular prostheses, commonly known as glass eyes or bionic eyes, aim to replace missing natural eyes, enhancing light sensitivity and providing a sense of vision for those with advanced vision loss.
Q: Can an ocular prosthesis restore normal vision?
A: While it doesn’t restore normal vision, an ocular prosthesis helps individuals with vision loss by improving light sensitivity and creating a semblance of visual perception.
Q: Are there functional benefits to using an ocular prosthesis?
A: Yes, ocular prostheses offer functional benefits, including improved light sensitivity and a sense of vision, enhancing the overall quality of life for individuals with visual impairments.
Materials and Crafting
Q: What materials are commonly used for crafting prosthetic eyes?
A: Modern prosthetic eyes are typically crafted from hard, plastic acrylic, providing a durable and realistic shell that fits over an ocular implant.
Q: How is the color of a prosthetic eye determined?
A: Ocularists work with patients to match the color and details of the prosthetic eye to the remaining natural eye, ensuring a realistic appearance.
Q: Can prosthetic eyes be customized for a natural look?
A: Yes, ocular prostheses are highly customizable, allowing for a natural look that closely resembles the appearance of the remaining natural eye.
Ocularist Specialization
Q: Who creates and fits ocular prostheses?
A: Ocularists are professionals who specialize in the fabrication and fitting of ocular prostheses, providing personalized solutions for individuals who have lost an eye due to trauma or illness.
Q: How does an ocularist determine the size of a prosthetic eye?
A: Ocularists take detailed measurements and work closely with patients to ensure the accurate sizing and fitting of the prosthetic eye for a comfortable and natural appearance.
Cosmetic Improvements
Q: Can an ocular prosthesis improve cosmetic appearance?
A: Yes, besides functional benefits, ocular prostheses contribute to cosmetic enhancements, positively impacting a patient’s overall appearance, health, and well-being.
Q: What role does an iris prosthesis play in cosmetic improvements?
A: Iris prostheses not only offer functional benefits like reduced glare but also contribute to cosmetic enhancements, playing a vital role in overall patient satisfaction and happiness.
Care and Maintenance
Q: How should one care for and clean an ocular prosthesis?
A: Ocular prostheses require regular cleaning with recommended solutions, and patients should follow the care instructions provided by their ocularist.
Q: Are there any specific precautions for protecting an ocular prosthesis?
A: Patients should avoid exposing ocular prostheses to extreme temperatures, chemicals, or sharp objects. Protective eyewear may be recommended in certain situations.
Adjustments and Adaptations
Q: Can the size or fit of a prosthetic eye be adjusted over time?
A: Yes, ocular prostheses can be adjusted or replaced to accommodate changes in the eye socket or surrounding facial structures over time.
Q: What if an ocular prosthesis feels uncomfortable or causes irritation?
A: Patients experiencing discomfort or irritation should promptly consult their ocularist for adjustments or possible replacements to ensure optimal comfort.
Long-Term Considerations
Q: How often should an ocular prosthesis be replaced?
A: The lifespan of an ocular prosthesis varies, but regular evaluations with an ocularist help determine when a replacement may be necessary due to wear or changes in the eye socket.
Q: Can children use ocular prostheses, and how often do they need replacements?
A: Yes, children can use ocular prostheses, and replacements may be more frequent due to growth. Regular check-ups with an ocularist help monitor and address any changes.
Emotional and Psychological Impact
Q: What emotional support is available for individuals adapting to an ocular prosthesis?
A: Ocularists often provide counseling and emotional support, helping individuals navigate the adaptation process and address any concerns or emotional challenges.
Q: How does wearing an ocular prosthesis impact self-esteem and confidence?
A: Wearing an ocular prosthesis can positively impact self-esteem and confidence, providing individuals with a restored appearance and helping them feel more comfortable in social situations.
Q: Are support groups available for individuals with ocular prostheses?
A: Yes, support groups and online communities offer valuable resources, allowing individuals to share experiences, advice, and emotional support throughout their journey with ocular prostheses.